Build Your Regenerative Medicine Authority Regenerative medicine authority starts with smart plans. Plus, you need strong leaders. Also, you must help patients. Therefore, this takes real work. The field needs great leaders today. Moreover, these leaders mix science with business. Thus, they help change patient care. Meanwhile, data proves the methods work. In fact, they
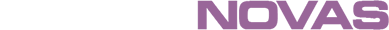
Despite progress in cardiovascular research, cardiac pathology continues to be one of the most common causes of morbidity and mortality in the world. Stem cell-based therapy has been recognized as an innovative strategy for the repair, regeneration and functional recovery of the myocardium, hence, once the animal research stage has been overcome, most clinical trials
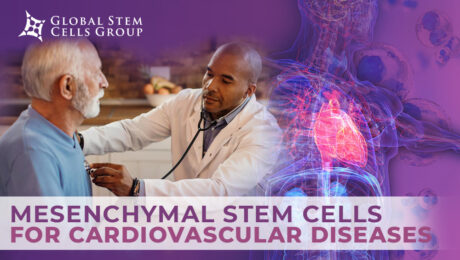
Atherosclerosis is the most common form of arterial occlusive disease in adults. About 15 percent of adults over 55 years of age suffer from critical ischemia, the most severe form of this disease. Due to the gradual aging of the population and the growing number of people in their third age group, a number of
In recent years, MSCs have been introduced as respectable candidates for regenerative medicine due to their pro-angiogenic, anti-apoptotic, and immunomodulatory attributes. A variety of human tissues can be used as a source of mesenchymal stem/stromal cells (MSCs), ranging from bone marrow (BM) to umbilical cord (UC). These cells are typically multipotent and can differentiate into
Stem cell therapy is a form of regenerative medicine designed to repair damaged cells within the body by reducing inflammation and modulating the immune system. This phenomenon makes stem cell therapy a viable treatment option for a variety of medical conditions. What is stem cell therapy? The term stem cell therapy refers to any treatment
The XXV Congreso Internacional de Medicina, Cirugia Estética y Obesidad will take place in CDMX, México on July 13,14 and 15, 2022. The International Society for Stem Cell Application (ISSCA) will be actively taking part in the congress. The ISSCA is a multidisciplinary community of physicians and scientists with a mission to advance the science,
Exosome therapy is the new buzz in the regenerative medicine industry because of how it can repair and regenerate your cells and tissues. Exosome therapy is safer compared to other cellular therapy because it’s a cell-free therapy with no risk of rejection. Exosome therapy will be beneficial to you if you’re dealing with conditions such
Mesenchymal Stem Cells (MSCs) are the most commonly used cells in stem cell therapy and regenerative medicine, due to their high and multi-potency. Mesenchymal Stem Cells (MSCs) can be isolated from different tissues in the body. In this article, you’ll be learning about culture-expanded MSCs, how MSCs can be expanded, The potency of MSCs and
Are you a physician that is currently utilizing adipose tissue, but is growing tired of the time-consuming, arduous procedure? Are you having problems finding reagents that allow you to isolate stem cells? If so, GCell might be the solution for you. What is GCell? GCell is a revolutionary new machine that holds the potential to
The International Society for Stem Cells Applications has officially announced and published its list of speakers for its 7th Annual Regenerative Medicine Symposium. The seventh event of its kind, it is another effort from the iSSCA to bring together a network of regenerative medicine practitioners from all over the world. At previous events, hundreds of
- 1
- 2